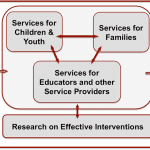
Each Category of Care will establish a nationwide standard for collecting translational data, a standard set of training, education and dissemination of information, and the ability to develop and monitor scientific investigative research.
- Prevention: Primary prevention entails preventing new injuries through education and encouragement to reduce high risk behaviors, engineering safer technologies, enforcement of safe practices, and evaluation of the impact of these measures. Secondary prevention involves reducing the severity of injuries, through improved medical practices. Tertiary prevention involves decreasing the frequency and severity of disability after an injury, via improved support structures in the post-acute setting.
- Acute Care: During this early period when minutes really count in terms of assessing injury severity, instituting effective neurosurgical and neurocritical care interventions and protecting the brain against any secondary injuries. What happens here effects everything that follows.
- “Mild” TBI: Millions of children, adolescents and young adults sustain a traumatic brain injury (TBI) per year. An overwhelming 90% of TBIs are classified as “mild”. “Mild” is merely a relative term, the clinical experience is not “mild.” Concussions are a subclass of “mild” TBI. The current status of “Mild TBI is lacking in many areas such as; education & awareness, medical, educational, sports/recreation systems under-prepared and ill-equipped, a lack of trained responsive systems (EMS, Primary Care, Clinics), and lack of services (Schools, Emergency Departments, and Pediatric Offices).
- Reintegration/ Long-Term Care: There is no systematic method for connecting children and their families with services within the school and community following TBI. There is an under-identification for special education. Annually 62,000 children are hospitalized for TBI, with approximately 19% needing special education supports.
- Adult Transition: Medical, Psychological and Rehabilitative services (PT, OT, Speech) are received through Special Education and end at age 21 with the end of school eligibility. The IEP process mandates a Transition Program to support the transition from school to post-secondary education or work. There is a lack of medical providers, PABI education, insurance coverage, and opportunity for informal social interactions. The PABI Plan addresses these problems by implicating a PABI Registry, an educational resource for physicians and other providers clarifying the course of PABI through development, impact of PABI trauma and medications on physical systems over time.
- Rural/ Tele-Health: The Scope of the problem is 80% of Rural Hospitals, without specialty staffing for neurologic emergencies, provide care for 54 million US citizens. About 17% of American children under the age of 18 live in rural areas. The proportion of rural children relative to urban children increased by 3% from 1990 to 2000. Aproximately 44% of American children live more than 200 miles from either a Children’s hospital (NACHRI) or a hospital with neurologic emergency care (this includes adult specialists). Even when emergent care is available, needed follow up care and rehabilitation would require a 4-hour commute. When funded, the SJBF state lead centers will provide expertise and coverage within a 200-mile radius for 42% of the US (including Hawaii, Alaska and Puerto Rico).
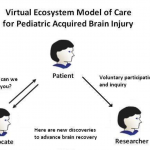
- The Virtual Center: A patient & family centered registry with an electronic health and personalized record portal integrated across life-ecosystems. This is online, up-to-date, and relevant content providing continual resources for children, families, and care providers. The Virtual Center promotes research, advances discovery speed, empowers patients & reaches communities, provides anonymous & highly linked care, and integrates data to inform public policy.
 JOIN THE REGISTRY
JOIN THE REGISTRY